Pain in the Brain
/“How can the brain think that the brain itself hurts (e.g., during a headache)? I don’t understand how the brain could even understand the concept of the brain hurting (i.e., have the machinery for concluding that the brain itself hurts), since the brain has no pain receptors. I guess stranger things have happened within abnormal psychology, though. Are headaches and migraines (excluding secondary headaches) essentially psychosomatic in nature?”
Before I answer your question, I need to say one important thing: ouch!
That’s right – as I sat down at my keyboard to answer your question, I stubbed my toe quite painfully on my desk. Fortunately, this is a great time to explain how the brain processes pain, which will help answer your question.
Sensing pain: A relay from stubbed toe to brain
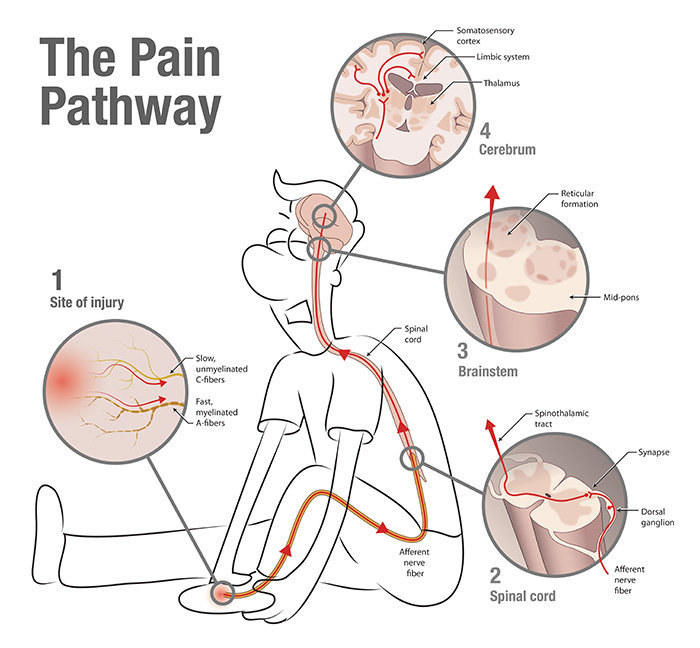
The path that a “this feels bad” signal travels going from a stubbed toe to the brain, where it is processed and made into the feeling of pain. Source: http://neurowiki2014.wikidot.com/group:pain
In your body, there are special sensory neurons called ‘nociceptors’ whose job it is to tell the body “this feels bad!” [Dubin 2010]. There are many different kinds of nociceptors; some detect harmful chemicals (like capsaicin, the ow-inducing ingredient in chili peppers), others harmful temperatures (like the surface of a hot stove), and still others detect bodily damage (like the strain that occurs in the tendons of your finger when you strike a piano key too forcefully). Nociceptors can also differ in the way they relay messages to the brain. Some, called A-fibers, have a fatty myelin sheath surrounding their long, arm-like axons that acts like insulation on a wire to help messages get to the brain quickly. These neurons were responsible for that first burst of pain in my big toe right when I stubbed it. Another type of nociceptor, called a C-fiber nociceptor, conducts signals much more slowly, but has many branches so that it reports to the brain from many different areas of the body. This type of nociceptor is associated with diffuse pain, and is likely to blame for that achey, burning feeling I have in the front of my foot right now.
Let’s follow the stubbed toe message along its way to the brain. First, the message passes from my foot, up my leg, and into my spinal cord, where it is relayed to neurons whose fibers climb all the way to the brain. Up through the brainstem these fibers go, traveling in bundles to the brain itself where the message ping-pongs between the thalamus, hypothalamus, and a number of other regions scientists are just beginning to parse [Almeida 2004]. The electrical communication between these regions gives rise to the feeling of pain.
From sensing to feeling
So what’s happening when it feels like your brain is hurting? You’re absolutely right that the brain has no nociceptors. In fact, nociceptors never develop in the brain; in embryos, the cells that are responsible for making nociceptors are different from the ones that make up the brain [Woolf 2007]. The brain is so insensitive to painful stimuli that neurosurgeons do not apply anaesthesia to the brain tissue they operate upon, allowing patients to be awake and completely responsive for the whole procedure. You can see this phenomenon for yourself in the video linked here. So if a brain is incapable of sending “this feels bad!” signals, why do headaches exist?
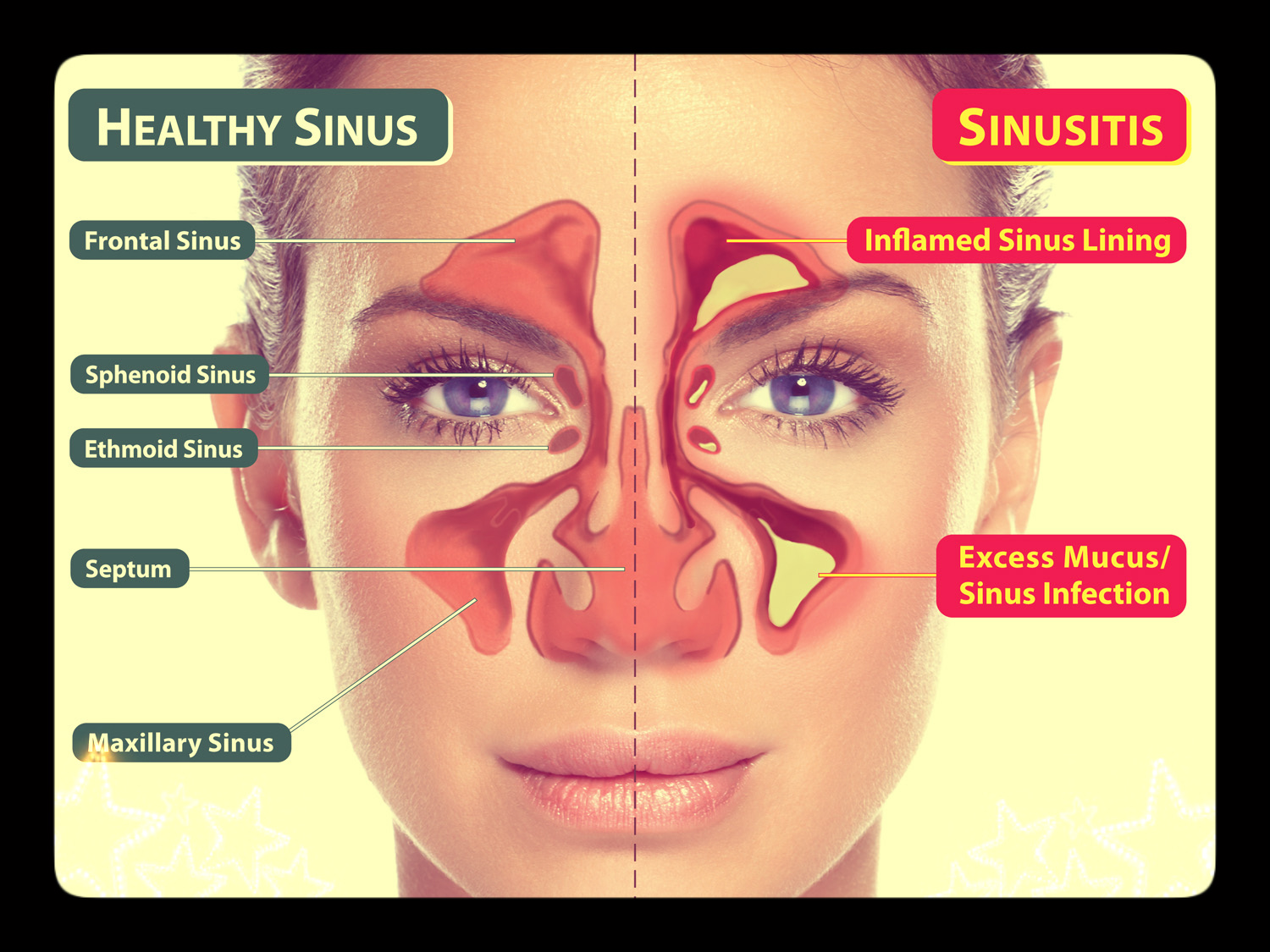
Although nociceptors embedded in your sinuses are in the front of your face, the brain can still interpret sinus pain as coming from the middle of your head. Source: http://ausfp.com/sinus-infection/
One answer is that the brain mistakenly identifies pain as coming from the middle of your head. Your brain can be bad at localizing certain types of head pain because there are so many different types of tissues in the head, and many of them are pretty bad at communicating where the hurt is happening. Fellow sinus infection sufferers will know what I’m talking about - inflammation of the spaces in just behind your forehead can feel like a knot of pain in the middle of your head.
As another example, consider brain freeze, the painful headache you get for a few seconds after eating ice cream too quickly. Why does it happen? Think back to a cold day spent outside: when the cold air first hits the blood vessels on your face, they eventually widen, giving you ruddy cheeks. The same thing happens when the top of your mouth is suddenly cooled - those blood vessels widen very suddenly, activating nociceptors in the roof of your mouth. Unfortunately, these nociceptors aren’t very precise in their description of where the pain is coming from, so they create the sensation of pain in the middle of head - a phenomenon that doctors call “referred pain” [Yankelowitz 2001, Andrews 2008]. You may have also heard of referred pain in the context of a heart attack - even though your heart is the damaged tissue, sufferers will often feel referred pain in their arm instead [Kosek 2003].
Finally, remember that your head is full of lots of tiny muscles. When these muscles are strained - say, because you were staring at your computer all day - the nociceptors embedded in these tissue types send pain signals. Many of these nociceptors are the type with a lot of branches, so that it can be hard for the brain to pinpoint exactly where the pain is coming from, and as a result the pain is difficult to localize.
Your brain also has the unfortunate ability to fabricate a sensation of pain when no nociceptors are active. To explain what I mean by this, it’s crucial to understand that “pain” (the feeling) doesn’t always result from “this feels bad” (the signal). Consider, for example, when you scrape your knee during a soccer game. You might be having so much fun that you don’t really feel the pain until after the game has ended and there is no longer something else distracting you from the pain. Well, your nociceptors were certainly sending “this feels bad” signals for the entire game, but your brain only processed the signals and created the feeling of pain later. This can go the other way, too - if you suffered from psychosomatic pain, you would feel pain even though your nociceptors are quiet. Your brain can even create feelings of pain in places that have no nociceptors - like a hand that has been missing for years [Flor 1995]. So, since pain doesn’t always mean nociceptors are active, it’s possible that so-called “brain pain” is just the accidental byproduct of a yet-unknown set of interacting brain regions.
An example of a scintillating scotoma, a type of visual aura that can precede a migraine that might be attributable to cortical spreading depression. Source: https://en.wikipedia.org/wiki/Scintillating_scotoma
Some scientists believe that migraines may be related to this kind of psychosomatic pain, but new evidence suggests that there is more to the story. Migraines and cluster headaches could be, in part, the brain ‘overreacting’ to otherwise humdrum nociceptor activity. That overreaction means that neurons along the pathway can convert the relayed pain signal from “this is tolerable” to “this is TERRIBLE!” . Another theory is that migraines occur when an aberrant electrical activity in brain accidentally stimulates nociceptors in surrounding blood vessels. This activity, a coupling of widespread neuron over-excitability followed by under-excitability, is “cortical spreading depression” (CSD) because of the way it propagates throughout parts of the cortex. Since this seems to affect areas of the cortex related to vision, the theory goes, this could explain why some migraine sufferers experience visual auras and dancing lights before the migraine starts.
According to the CSD theory, this could kick off a chain of events whereby neurons induce neighboring cells called glia to release inflammatory factors that force blood vessels to narrow, stimulating a relay of painful headache signals. So, to summarize, there could be a double whammy in the heads of people suffering debilitating headaches: neurons that are overly sensitive to normal sensations, and a brain that massively over-interprets where and how painful those sensations are.
Scientists will need to investigate many more questions before they can truly explain why migraines happen. In most cases, however, it's safe to assume that your headache is the result of your brain’s interpretation (or misinterpretation) of the activation pattern of nociceptors in your head’s muscles and blood vessels. I hope that helps!
Sources
Almeida, Tatiana F., Suely Roizenblatt, and Sergio Tufik. "Afferent pain pathways: a neuroanatomical review." Brain research 1000.1 (2004): 40-56.
Scientific American Mind, 1555–2284, 2008, Vol. 19, Issue 1. "Brain Freeze." Andrews, Mark A., Lake Erie College of Osteopathic Medicine.
Dubin, Adrienne E., and Ardem Patapoutian. "Nociceptors: the sensors of the pain pathway." The Journal of clinical investigation 120.11 (2010): 3760.
Flor, H., et. al. (1995). Phantom-limb pain as a perceptual correlate of cortical reorganization following arm amputation. Nature No. 6531, pp. 482-484.
Kosek, E., et. al. (2003) Perceptual integration of intramuscular electrical stimulation in the focal and the referred pain area in healthy humans, Pain, Volume 105, Issues 1–2, Pages 125-131
Moskowitz, M. A., et. al., (1989) Pain mechanisms underlying vascular headaches, Revue Neurologique, Volume 3, Issue 145, Pages 181–193
Purves, D., et.al (2004). Neuroscience. Massachusetts: Sinauer Associates, Inc.
Slavin, KV, (2011) Peripheral Nerve Stimulation, Prog Neurol Surg, Volume 24, Pages 16–26
Strassman, A.M., et. al.. (1996) Sensitization of meningeal sensory neurons and the origin of headaches. Nature 384, Pages 560 - 564
Vania Apkarian, A. , et. al. (2005). Human brain mechanisms of pain perception and regulation in health and disease, European Journal of Pain, Volume 9, Issue 4, Pages 463-484
Woolf, C., et. al. (2007) Nociceptors—Noxious Stimulus Detectors. Neuron, Volume 55, Issue 3, Pages 353-364
Yankelowitz, SK.; Zagami, AS., (2001) Cold-stimulus headache, Cephalalgia, Volume 10, Issue 21