Ask a Neuroscientist: Restless Legs Syndrome
/“I have a family member who finds it very difficult to fall asleep because of restlessness in his left leg. Is restless leg syndrome a neurological disorder? What could be the root cause and is there any cure?”
I’m sorry for your family member! For those who haven’t heard of it, restless leg syndrome (RLS) is a persistent urge to move the legs that specifically comes on at night when you’re trying to go to sleep. Sufferers, who make up perhaps 5% of the population, can be so disturbed by the need to move their legs that they can’t fall asleep and become chronically sleep deprived. I jumped on your question because RLS runs in my family and in recent years I've had occasional mild symptoms myself. I have to tell you, it is a really strange sensation. I get an indescribable discomfort around my hip, and there's just no choice but to shake my leg around (it's always the right leg) until it goes away. Meanwhile, I’m going “Why am I doing this?”
I must also confess that I fell deep into a rabbit hole of RLS and related research in writing this article. You are right, this is a neurological disorder, and we have some tantalizing clues about its cause--but there are far more questions than answers at this point. I’m going to try to sketch how I understand the current evidence, but I have to say up front that this picture is tentative and research is ongoing.
One might imagine that this disorder could be caused by the peripheral nervous system that directly controls the execution of movements, but surprisingly, it originates in the brain. One piece of evidence for this is the fact that a class of drugs sometimes used to treat RLS are dopaminergic agents. These drugs stimulate receptors for the neurotransmitter dopamine, which is produced in a brain structure called the substantia nigra and transmitted to numerous other brain areas.
Dopaminergic neurons in the substantia nigra are critical both for movement generation and for cognitive functions like reward processing. You may be familiar with the role of dopamine in health because of two very different diseases: In Parkinson’s disease, neurodegeneration of dopaminergic neurons is thought to be responsible for patients’ difficulties in initiating movements, and is treated by stimulating dopamine receptors to make up for their loss. And there seems to be some role for dopamine in schizophrenia because antipsychotic medications block dopamine receptors.
I don’t know about you, but my head was spinning from how different these functions of dopamine are. How can a single nucleus do these wildly different things?
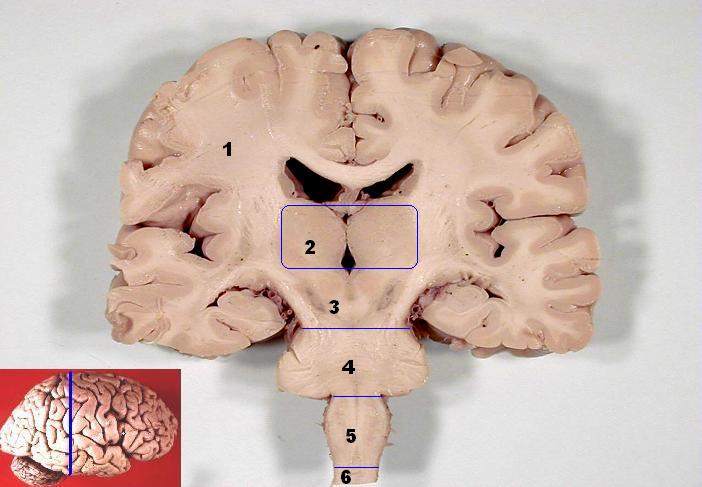
While dopamine signaling changes play some kind of role in RLS, they may not be the only or the primary cause of RLS; these changes could be downstream of some other cause. One such possibly-more-primary problem that researchers are actively exploring is iron metabolism. Iron is a nutrient we get from our diet that is critical for cellular metabolism. It’s present throughout the brain, but interestingly, it is enriched in the substantia nigra (SN). The substantia nigra gets its Latin name from its black color: if you ever get a chance to see slices of human brain tissue, look for the little spot of black pigment deep inside the brain. That’s the SN. The blackness of this nucleus comes from the high density there of neuromelanin, a pigment related to the melanin that colors our skin. In the brain, neuromelanin performs the function of storing iron and other metals; if they aren’t “buffered” by neuromelanin, they can form free radicals that go around stealing electrons from other molecules and causing oxidative damage.
Human brain frontal (coronal) section. Can you spot the substantia nigra? Hint: it's 2 (bilateral) regions that are substantially darker than the tissue that surrounds them.
But why is iron enriched in the SN in the first place? The best answer I could find for this is that iron is necessary for a step in the dopamine synthesis pathway. So these substantia nigra cells are making tons of dopamine, which requires iron, but storing a lot of iron requires careful regulation because if it isn’t chaperoned carefully by neuromelanin and associated proteins, it can cause oxidative stress.
Circling back to restless leg syndrome, another treatment that is effective for at least some patients is… iron supplementation! In RLS sufferers, iron is sometimes-but-not-always depleted in the substantia nigra, even if their blood doesn’t show signs of iron deficiency. To add to the intrigue, we know that RLS is genetic because it’s passed down in families, and some of the gene variants that have been discovered to increase the risk of developing RLS are involved in regulating iron metabolism.
Hence, both dopamine and iron seem to play a role, and both are targets of current treatments for RLS. But as far as the mechanism of pathogenesis: so many questions, so few answers.
To return to your relative, he should absolutely be talking to a doctor about possible treatments, not least because RLS can be caused by other conditions. Also, in my experience (and according to the NIH), stress is a big trigger, so whatever your family member can do to deal with stress effectively can help lower the chance of experiencing symptoms. I'm sure you've heard plenty about stress, but one approach to stress that I really like is presented entertainingly in this TED talk by Stanford psychologist Kelly McGonigal and in this publicly available and concise literature review. You'll be completely unsurprised to hear that getting regular exercise can also help, as can avoiding caffeine: nothing magical, just the usual old virtues.